Granulomatosis with Polyangiitis (GPA) is a rare but serious condition that belongs to a group of diseases known as vasculitis.
Vasculitis refers to the inflammation of blood vessels, and in the case of GPA, the inflammation primarily affects small- and medium-sized blood vessels.
This condition can impact various organs, including the kidneys, lungs, sinuses, and upper respiratory tract, and if left untreated, it can lead to severe complications.
Understanding GPA, its symptoms, diagnostic methods, and treatment options is crucial for managing the disease and improving outcomes for those affected.
- What is Granulomatosis with Polyangiitis?
- Causes and Risk Factors of GPA
- Known Risk Factors:
- Symptoms of Granulomatosis with Polyangiitis
- General Symptoms:
- Respiratory Symptoms:
- Kidney Symptoms:
- Other Symptoms:
- Diagnosing Granulomatosis with Polyangiitis
- Diagnostic Methods:
- Treatment for Granulomatosis with Polyangiitis
- Common Treatment Options:
- Long-Term Management:
- Outlook for People with Granulomatosis with Polyangiitis
- Conclusion
- People May Ask
- 1. What causes Granulomatosis with Polyangiitis?
- 2. How is GPA diagnosed?
- 3. Can Granulomatosis with Polyangiitis be cured?
- 4. What is the prognosis for someone with GPA?
- 5. Is GPA an autoimmune disease?
What is Granulomatosis with Polyangiitis?
Granulomatosis with Polyangiitis (GPA) is a type of autoimmune disease where the immune system mistakenly attacks healthy blood vessels, causing inflammation.
This inflammation can damage tissues and organs, leading to a wide range of symptoms. GPA is often associated with the presence of anti-neutrophil cytoplasmic antibodies (ANCA), which are specific antibodies that target certain white blood cells, leading to blood vessel damage.
While it can affect any organ, it most commonly impacts the lungs, kidneys, and upper respiratory tract.
MUST READ: Pacemakers vs. Implantable Defibrillators: What You Need to Know
Causes and Risk Factors of GPA
The exact cause of GPA is still unknown, but it is believed to result from a combination of genetic and environmental factors.
People with a family history of autoimmune diseases are at a higher risk, and certain infections or environmental exposures may trigger the condition in those who are genetically predisposed.
Known Risk Factors:
- Age: GPA typically affects individuals between the ages of 40 and 60, though it can occur at any age.
- Gender: The disease affects men and women equally, but some studies suggest that it may be more severe in men.
- Genetic predisposition: Certain genetic factors, such as specific variations of the HLA-DRB1 gene, may increase the risk of developing GPA.
- Infections and environmental exposures: Although no specific environmental triggers have been identified, some researchers suspect that infections or exposure to certain chemicals may play a role.
Symptoms of Granulomatosis with Polyangiitis
The symptoms of GPA can vary widely depending on which organs are affected. The disease often develops gradually and can lead to severe damage if left untreated. Common symptoms include:
General Symptoms:
- Fatigue and unexplained weight loss.
- Fever and muscle aches.
- Night sweats.
Respiratory Symptoms:
- Chronic sinusitis (inflammation of the sinuses).
- Nasal ulcers and bleeding.
- Cough, often accompanied by blood-tinged sputum.
- Shortness of breath or chest pain, especially if the lungs are involved.
Kidney Symptoms:
- Kidney dysfunction and high blood pressure.
- Presence of blood or protein in the urine.
- Edema (swelling) in the legs or ankles.
Other Symptoms:
- Joint pain and swelling.
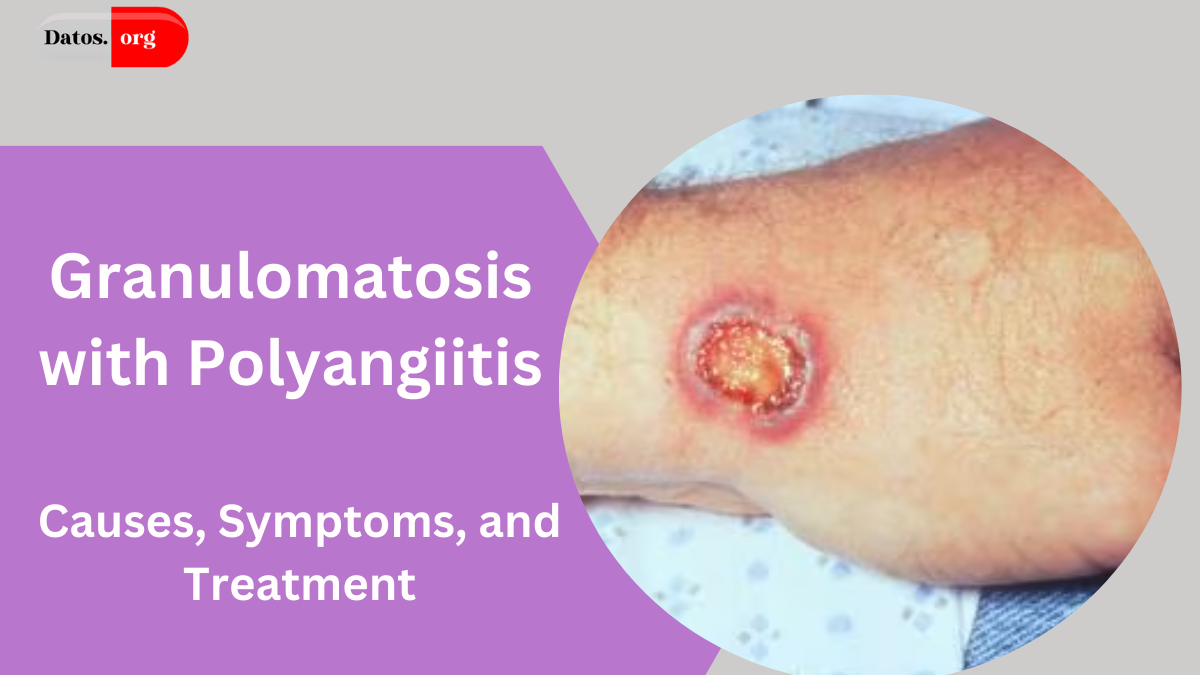
- Skin rashes or lesions.
- Hearing loss or ear infections when the disease affects the ears.
Because the symptoms of GPA can overlap with those of other conditions, it’s important to see a doctor for a thorough evaluation if any of these signs appear.
Diagnosing Granulomatosis with Polyangiitis
Diagnosing GPA can be challenging due to its wide range of symptoms and similarity to other conditions. A combination of clinical evaluation, laboratory tests, and imaging studies is often required.
Diagnostic Methods:
- Blood tests: The presence of ANCA (anti-neutrophil cytoplasmic antibodies) is a key marker in diagnosing GPA. However, not all patients with GPA will test positive for ANCA.
- Urine tests: Urinalysis may reveal the presence of blood or protein, which is common in kidney involvement.
- Imaging: Chest X-rays, CT scans, or MRI scans can help detect lung involvement, sinus abnormalities, or other organ damage.
- Biopsy: In some cases, a tissue biopsy may be performed on an affected organ, such as the kidneys or lungs, to confirm the diagnosis and assess the degree of damage.
Treatment for Granulomatosis with Polyangiitis
While there is currently no cure for GPA, treatment can help manage symptoms, reduce inflammation, and prevent organ damage.
The primary goal of treatment is to induce remission, where symptoms subside, and the disease activity is minimised.
Treatment often involves medications to suppress the immune system and address the inflammation.
Common Treatment Options:
- Corticosteroids: These are often used in combination with other immunosuppressive drugs to reduce inflammation. Prednisone is commonly prescribed to help manage flare-ups.
- Immunosuppressive drugs: Drugs like cyclophosphamide, methotrexate, or azathioprine may be used to suppress the immune system and reduce the activity of the disease.
- Rituximab: This biologic medication may be used for more severe cases or when other treatments don’t work. It targets B-cells, a type of white blood cell involved in the immune response.
- Plasma exchange (plasmapheresis): In cases of severe kidney involvement or life-threatening symptoms, plasma exchange may be used to remove harmful antibodies from the bloodstream.
Long-Term Management:
After achieving remission, patients typically continue on lower doses of immunosuppressive drugs to maintain the remission and prevent flare-ups. Regular follow-up visits and monitoring are important to assess kidney function, lung health, and other affected organs.
Outlook for People with Granulomatosis with Polyangiitis
With early diagnosis and appropriate treatment, many individuals with GPA can lead relatively normal lives. However, the disease can be life-threatening if left untreated, especially when it affects vital organs such as the kidneys or lungs. Ongoing medical care and monitoring are crucial to managing the disease and preventing long-term complications.
Conclusion
Granulomatosis with Polyangiitis (GPA) is a rare but serious condition that can affect various organs in the body, particularly the kidneys, lungs, and upper respiratory tract. With appropriate treatment, such as immunosuppressive therapy and corticosteroids, most people with GPA can manage their symptoms and prevent significant organ damage. Early diagnosis and treatment are key to improving long-term outcomes, so it is vital to seek medical attention if any concerning symptoms arise.
People May Ask
1. What causes Granulomatosis with Polyangiitis?
The exact cause of GPA is unknown, but it is believed to result from a combination of genetic and environmental factors, including infections or exposure to chemicals that may trigger the immune system’s attack on blood vessels.
2. How is GPA diagnosed?
GPA is diagnosed through a combination of blood tests for ANCA antibodies, urine tests, imaging studies, and in some cases, a biopsy of an affected organ like the kidneys or lungs.
3. Can Granulomatosis with Polyangiitis be cured?
There is no cure for GPA, but treatment can help control symptoms and induce remission. With appropriate therapy, most people can live a relatively normal life.
4. What is the prognosis for someone with GPA?
The prognosis depends on how early the disease is diagnosed and treated. With proper care, many individuals can manage GPA and avoid serious complications. However, without treatment, GPA can be fatal.
5. Is GPA an autoimmune disease?
Yes, GPA is an autoimmune disorder in which the immune system attacks healthy blood vessels, causing inflammation and damage to various organs in the body.
Click here to learn more.